Background
Allogeneic hematopoietic stem cell transplantation (HSCT) as consolidation therapy is considered a curative option for acute myeloid leukemia (AML) in complete remission (CR) to prevent relapse. Many studies have investigated the optimal conditioning intensity, comparing reduced-intensity conditioning regimen (RIC) and myeloablative conditioning regimen (MAC) for patients with AML in CR. However, inconsistent results have been observed, possibly due to selection biases and significant heterogeneous treatment effects when focusing on average treatment effect. Some studies have attempted to assess treatment effects in specific subgroups, highlighting the heterogeneity conditioning intensity's impact. However, these analyses typically examined one factor at a time, overlooking potential multiple-factor combinations that might contribute to such heterogeneity.To address these limitations and surpass conventional comparison studies and subgroup analyses, machine-learning methods for group identification have been developed. In this study, we aimed to identify patient groups in which MAC or RIC had a superior PFS in patients with AML in CR using a machine-learning approach.
Methods
Our study included 3273 patients aged 40-69 years with AML in CR from the TRUMP2. These patients were divided into training (N=2020) and validation cohorts (N=1253). In the training cohort, we employed a group identification model to identify patient subsets. Preprocessing of variables was performed to ensure the ease of use in clinical practice. We modeled the magnitude of interaction between treatment and covariates without the main effect of covariates, thus leading to the construction of a scoring system that measures the individualized-treatment effect. The objective variable was set as 1-year PFS, and the interaction effects between treatment and covariates were estimated using a regression model with propensity score weight and LASSO regularization. The sum of the interaction term between treatment and covariates was defined as the “Conditioning Intensity Score”. Patients were categorized into high-score and low-score groups using a cut-off level of median in patients who received RIC. Subsequently, in the validation cohort, we estimated the average treatment effect of RIC compared to MAC for each group with hazard ratios (HR) using inverse treatment probability weight analysis.
Results
In the training cohort, the median age was 55 years (IQR, 48-61 years), with 1110 (55%) male patients. Among them, 666 (33%) received RIC, while the others underwent MAC. Conditioning Intensity Model was developed and consistent with followings; age over 49 (1.4 points), age over 49 and male (0.8 points), age over 49 and poor karyotype (0.5 point), age over 49 and cord blood transplantation (0.9 points), poor karyotype (-1.6 points), poor karyotype and primary induction failure (8.0 points), poor karyotype and bone marrow transplantation (-5.3 points), cord blood transplantation and hematopoietic cell transplant comorbidity index over 2 (2.1 points) and cord blood transplantation and extra bone marrow involvement (-8.6 points). The cut-off level was set as 2.2. The weighted HR of RIC on 1-year PFS was 0.56 (95%CI; 0.40-0.79, p < 0.001) in the high-score group and 1.23 (95%CI: 0.97- 1.57, p=0.094) in the low-score group.
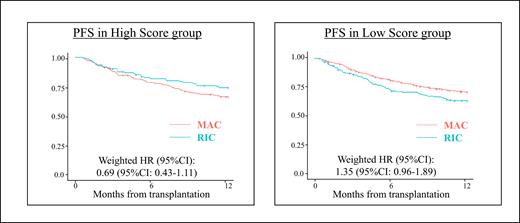
In the entire validation cohort, there were no significant differences in PFS between the RIC and MAC (67.7% [95% CI: 62.1-70.3%] in the RIC group vs. 70.3% [95% CI: 67.2-73.1%] in the MAC group, P=0.318). Patients were divided into two groups based on Conditioning Intensity Score. In the high-score group, the 1-year PFS was 73.9% (95% CI: 65.0-80.9%) in the RIC group vs. 66.2% (95% CI: 58.3-73.0%) in the MAC group ( P=0.181), with a weighted HR of 0.69 (95% CI: 0.43-1.11) for PFS in the RIC group compared to that the MAC group ( P=0.125) (Figure left). Conversely, in the low-score group, the 1-year PFS was 63.7% (95% CI: 56.3-70.2%) in the RIC group vs. 71.2% (95% CI: 67.8-74.2%) in the MAC group ( P=0.031), with a weighted HR of 1.35 (95% CI: 0.96-1.89) in the RIC group compared to the MAC group (log-rank P=0.086) (Figure right).
Conclusion
In conclusion, we have demonstrated the feasibility of utilizing a machine learning method for subgroup identification of conditioning regimens in patients with AML in CR. This established model holds promise for designing patient-specific regimens.
Disclosures
Kondo:Asahi Kasei Pharmaceutica,Chugai Pharma, MSD Pharmaceutical, Dainippon Sumitomo Pharma, Otsuka Pharmaceutical: Honoraria, Research Funding. Harada:Nippon Shinyaku: Research Funding. Doki:Janssen Pharmaceutical K.K.: Honoraria; Novartis Pharma K.K.: Honoraria. Tanaka:Otsuka Pharmaceutical: Speakers Bureau; MSD: Speakers Bureau; Kyowa-Kirin: Speakers Bureau; Daiichi Sankyo: Speakers Bureau; Chugai Pharmaceutical: Speakers Bureau; Astellas Phrama: Speakers Bureau; Asahi Kasei Pharma: Speakers Bureau; Abbvie: Speakers Bureau; Sumitomo Pharma: Speakers Bureau; Pfizer: Speakers Bureau. Kanda:Taiho Pharmaceutical: Research Funding; Bristol Myers Squibb: Speakers Bureau; Novartis: Speakers Bureau; Chugai Pharmaceutical: Research Funding, Speakers Bureau; Pfizer: Speakers Bureau; Sanofi: Speakers Bureau; Janssen Pharmaceutical: Speakers Bureau; Kyowa Kirin: Research Funding, Speakers Bureau; MSD: Speakers Bureau; Saitama Hokeni Kyokai: Speakers Bureau; Daiichi Sankyo: Research Funding, Speakers Bureau; Asahi Kasei Pharma: Research Funding, Speakers Bureau; Meiji Seika Pharma: Speakers Bureau; Takeda Pharmaceutical: Research Funding, Speakers Bureau; Amgen: Speakers Bureau; Sumitomo Pharma: Research Funding, Speakers Bureau; Human Life CORD: Speakers Bureau; AstraZeneca: Speakers Bureau; Otsuka Pharmaceutical: Research Funding, Speakers Bureau; Japan Blood Products Organization: Research Funding, Speakers Bureau; CSL Behring: Speakers Bureau; AbbVie: Research Funding, Speakers Bureau; Towa Pharma: Speakers Bureau; Nippon Shinyaku: Speakers Bureau; FUJIFILM Wako Pure Chemical: Speakers Bureau; Wakunaga Pharmaceutical: Speakers Bureau; Eisai: Research Funding, Speakers Bureau; Precision: Speakers Bureau; Alexion Pharma: Speakers Bureau; Shionogi Pharma: Research Funding; Nippon Kayaku: Research Funding; JCR Pharmaceuticals: Research Funding. Sawa:Sanofi: Honoraria; Janssen: Honoraria. Fukushima:Janssen: Honoraria. Kanda:Amgen: Ended employment in the past 24 months, Honoraria; Janssen Pharmaceutical K.K.: Honoraria; Novartis Pharma K.K.: Honoraria; Sanofi K.K.: Honoraria; AbbVie Pharma: Honoraria; Megakaryon Co.: Honoraria; Eisai Co.: Research Funding. Atsuta:Novartis Pharma KK: Speakers Bureau; Otsuka Pharmaceutical Co., Ltd: Speakers Bureau; CHUGAI PHARMACEUTICAL CO., LTD.: Speakers Bureau; JCR Pharmaceuticals Co., Ltd.: Consultancy; Meiji Seika Pharma Co, Ltd.: Honoraria.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal